What is the CPT code for a phone consultation?
Codes for phone consultations with physician extenders, who are usually nurses, NPs, or PAs, usually correspond with a bill that is less than the bill for phone conversations with your doctor. 1 98966 phone call 5 to 10 minutes of medical discussion 98967 phone call 11 to 20 minutes of medical discussion
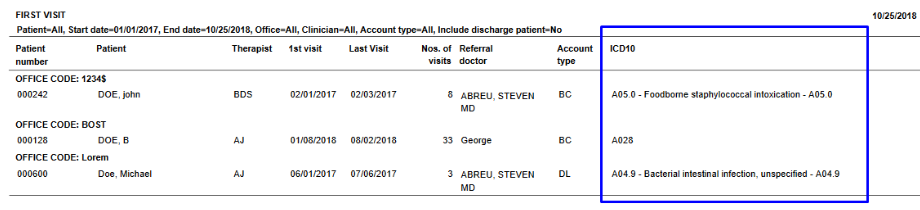
What is the ICD 10 code for consultation?
2018/2019 ICD-10-CM Diagnosis Code Z71.0. Person encountering health services to consult on behalf of another person. Z71.0 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
Can I Bill more than one code for a phone call?
If the call lasts longer than 30 minutes, you can use more than one of these codes. For example, a 45-minute call can be billed as both 98968 and 98967. To fulfill medical necessity, the following criteria must be met when billing 98966-98968: The call must be initiated by the established client or their parent/guardian if they’re a minor.
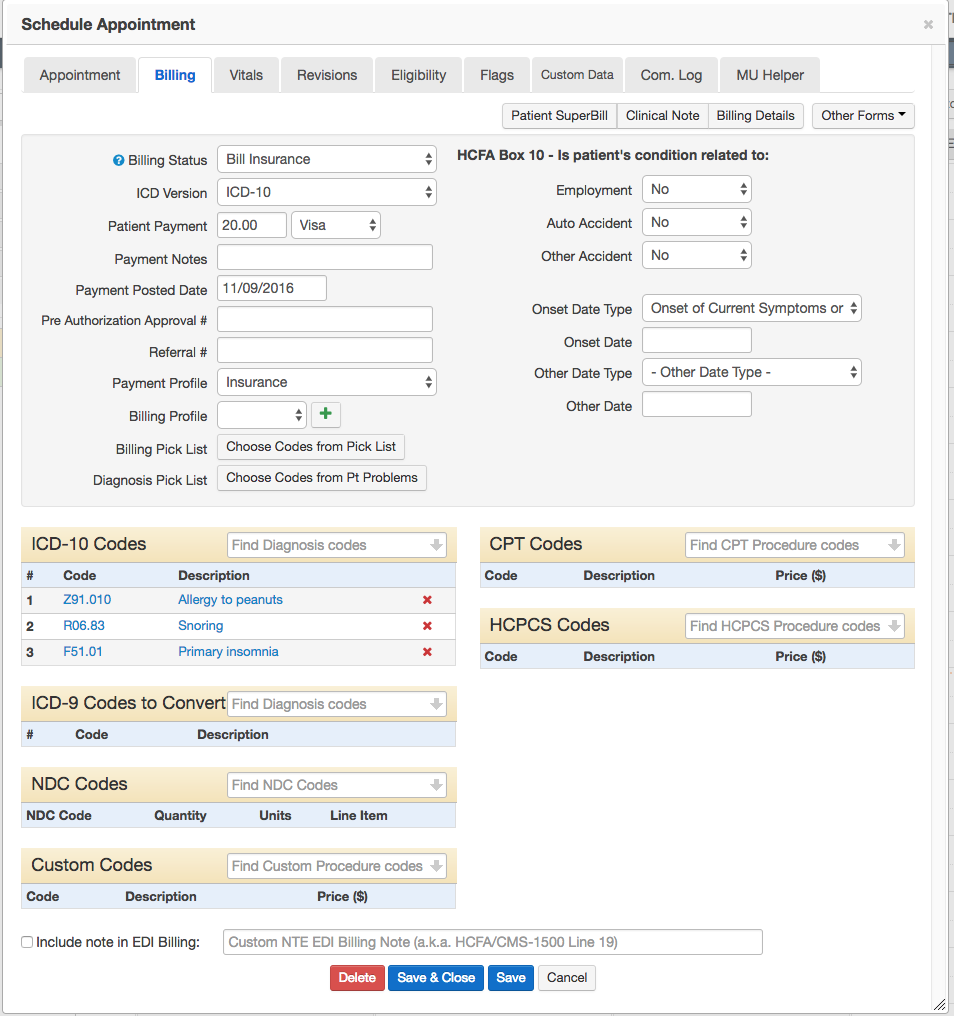
What are common procedure coding system (HCPCS) codes?
For Medicare patients, these are known as Healthcare Common Procedure Coding System (HCPCS) codes . Every procedure and service you receive from a medical provider uses these codes, which are required along with your bill.
When will the Z71.9 ICd 10 be released?
What is Z71 in medical?
What is a Z00-Z99?
About this website
2022 ICD-10-CM Diagnosis Code Z01.89
Note. Z codes represent reasons for encounters. A corresponding procedure code must accompany a Z code if a procedure is performed. Categories Z00-Z99 are provided for occasions when circumstances other than a disease, injury or external cause classifiable to categories A00-Y89 are recorded as 'diagnoses' or 'problems'.This can arise in two main ways:
ICD-10-CM Code Z71.9 - Counseling, unspecified
This is the official approximate match mapping between ICD9 and ICD10, as provided by the General Equivalency mapping crosswalk. This means that while there is no exact mapping between this ICD10 code Z71.9 and a single ICD9 code, V65.9 is an approximate match for comparison and conversion purposes.
Z71.9 COUNSELING, UNSPECIFIED - 2022 ICD-10-CM - Health Providers Data
Diagnosis Code: Z71.9 Short Description: Counseling, unspecified Long Description: Counseling, unspecified The code Z71.9 is VALID for claim submission. Code Classification: Factors influencing health status and contact with health services (Z00–Z99)
2022 ICD-10-CM Diagnosis Code Z71.85
Note. Z codes represent reasons for encounters. A corresponding procedure code must accompany a Z code if a procedure is performed. Categories Z00-Z99 are provided for occasions when circumstances other than a disease, injury or external cause classifiable to categories A00-Y89 are recorded as 'diagnoses' or 'problems'.This can arise in two main ways:
2022 ICD-10-CM Code Z71.9 - Counseling, unspecified
Z71.9 is a billable diagnosis code used to specify a medical diagnosis of counseling, unspecified. The code Z71.9 is valid during the fiscal year 2022 from October 01, 2021 through September 30, 2022 for the submission of HIPAA-covered transactions.
When will the Z71.0 ICd 10 be released?
The 2022 edition of ICD-10-CM Z71.0 became effective on October 1, 2021.
What is Z71 in medical?
Z71- Persons encountering health services for other counseling and medical advice , not elsewhere classified
What is a Z00-Z99?
Categories Z00-Z99 are provided for occasions when circumstances other than a disease, injury or external cause classifiable to categories A00 -Y89 are recorded as 'diagnoses' or 'problems'. This can arise in two main ways:
What is the code for a telephonic visit?
This visit would now revert to a telephonic visit, again, codes, 99441-99443, and time would need to be documented to enable the provider to choose the correct code. These are time-based codes.
When will CMS update telehealth?
Original story posted on: April 13, 2020. As CMS continues to update their policies on telehealth during the COVID-19 pandemic and the Public Health Emergency, ICD10monitor is here to continue to keep you informed on these changes.
Can a doctor use a cell phone for video chat?
ANSWER: No. The provider must use telecommunication application, which mandates audio and visual, under Waiver 1135. They can use their smart phone or cell phone for the doctor-to-patient phone calls, and most cell phones have a video chat option (i.e. FaceTime, Skype, Google Duo, Facebook Video Chat). I know this is causing confusion.
Does the Social Security Act require video chat?
ANSWER: Since the main focus of the visit was done without video chat capabilities, as mandated by the new waiver in Section 1135 (b) of the Social Security Act explicitly allowing the U.S. Department of Health and Human Services (HHS) Secretary to authorize use of telephones that have audio and video capabilities for the furnishing of Medicare telehealth services during the COVID-19 Public Health Emergency..
What is the code for a physician extender?
Codes for phone consultations with physician extenders, who are usually nurses, NPs, or PAs, usually correspond with a bill that is less than the bill for phone conversations with your doctor. 1 . 98966 phone call 5 to 10 minutes of medical discussion. 98967 phone call 11 to 20 minutes of medical discussion.
How long is a 99441 call?
1 . 99441 phone call 5 to 10 minutes of medical discussion. 99442 phone call 11 to 20 minutes of medical discussion. 99443 phone call 21 to 30 minutes of medical discussion.
What is the AMA code for email?
No matter the format, the AMA designates them with two codes: one for your doctor and the other for a physician extender. 1 . 99444 Email or some other online service to discuss a medical problem with a physician.
Can you see a doctor through telemedicine?
As telemedicine is becoming more common, people like you often have the option to "see' the doctor using telemedicine or virtual care, which can be convenient if you don't want to spend too much time at the doctor's office.
Do insurance companies pay for patient calls?
Recently, some private insurance companies have begun to pay for patient-to-provider phone calls, especially when the calls are prolonged and when medical decisions are made. Nevertheless, you may be billed for the whole cost, or you may have to pay a co-pay. While you shouldn't hesitate to call your doctor, you should familiarize yourself ...
Does insurance pay for phone and online medical services?
While there are codes for phone and online medical services, this doesn't mean that your insurer will pay for them. Many insurance companies are adding coverage for telephone and online health services because it may prevent you from having to go through an unnecessary emergency room visit—which may be both inconvenient and costly. 3
Where is the place of service code for telehealth sessions?
The place of service code for most sessions are set in an office as “11” but for telehealth sessions the place of service code is “2”. The place of service code is posted on the CMS1500 under Box 24 section B.
What is the correct place of service code for mental health?
Instead, you want to utilize normal mental health procedure codes listed below and use the appropriate CPT code modifier (95 or GT) with the correct place of service code (02).
What is CPT code modifier?
CPT Code Modifier GT describes Synchronous Telemedicine Services provided in real time in the same manner as a typical face-to-face session.
What is telehealth billing?
Telehealth billing for therapists is complex, requiring the correct medical claims coding cpt codes, modifiers, and place of service code. Our exhaustive guide to telehealth billing for therapists will teach you how to code your mental health insurance claims for telehealth billing as the process to ensure you get paid every time. We will also go through major insurance brands like Medicare, Medicaid, etc, and their telehealth billing guidelines.
How to get reimbursed for telehealth therapy?
To ensure you get reimbursed for providing telehealth psychotherapy, always call each client’s insurance plan and ask about approval for telehealth therapy.
Why do therapists need telehealth?
Telehealth billing for therapists is an obvious need. Providers want to help clients who are unable to attend in person therapy for whatever reason: fear, disability, distance, or simply for ease of scheduling. For whatever reason, insurance companies have pushed back against telehealth for psychotherapy. Our guide will show you how ...
What to do if you are not sure what CPT code to use?
If you’re not sure which CPT code to use, consider hiring our billing service to demystify the process.
What is the CPT code for a call?
Billing for Phone Calls with CPT Codes 98966, 98967, and 98968. By TherapyNotes, LLC on September 19, 2018. As a therapist, you expect to receive phone calls from clients. Many practitioners don't charge for short calls, especially if they're for scheduling purposes, but what do you do when a phone call from a client becomes more complex ...
What is the CPT code for YouTube?
You may be able to use CPT codes 98966-98968. If playback doesn't begin shortly, try restarting your device. Videos you watch may be added to the TV's watch history and influence TV recommendations. To avoid this, cancel and sign in to YouTube on your computer.
What is the best way to do consent for services?
The best place to do this is on the Consent for Services form you have your clients sign. Make part of this form your out-of-session contact policy, stating that clients will be liable for all charges not covered by insurance. Naturally, this will exclude Qualified Medicare Beneficiaries and some Medicaid clients, who can’t be billed for anything, but it will cover your bases with all other clients.
What is the CPT code for a non-physician?
According to the CPT manual, the 98966, 98967, and 98968 CPT codes are used for " telephone assessment and management service provided by a qualified non-physician health care professional to an established client, parent or guardian ."
How to bill insurance company after phone call?
After each phone call that you want to bill, submit the claim to the insurance company for reimbursement. Even if it seems likely to be denied, this will prove to your client that you attempted reimbursement and thus have a valid reason for charging them directly.
How long is a 98968 call?
98968: 21-30 minutes. If the call lasts longer than 30 minutes, you can use more than one of these codes. For example, a 45-minute call can be billed as both 98968 and 98967.
Who initiates a call with a minor?
The call must be initiated by the established client or their parent/guardian if they’re a minor.
What is the code for online evaluation?
Code 99444 – The code used for online evaluation and management services. It helps in telling the payer that the consultation has happened online and there aren’t much details about the treatment and all. This in turns helps the healthcare providers and insurance companies to keep a record.
What is telemedicine used for?
Telemedicine is used for monitoring people in the rural and urban areas who are suffering from chronic illness. The standard of the telemedicine is the same as in person treatment. It is also safe and effective for the patients and is intended to be inexpensive and convenient. It is not a new concept. Many specialists and medical service providers have already adopted and implemented in their medical practices.
What is GT modifier?
The GT Modifier helps in keeping a track and lets them know that the visit has taken place virtually on this telemedicine platform. This in turns helps in keeping and maintaining a record.
What is the code for an audio only encounter?
Whether physicians report the audio-only encounter to a private payer as an office visit (99201-99215) or telephone E/M service (99441-99443) will depend on what the physician is able to document from the encounter. Physicians should report the code that appropriately reflects services rendered.
What is the UHC code for a medical office visit?
Physicians should report the code that appropriately reflects services rendered. UHC will allow office visits (99201-99215) via audio-only for Medicaid and commercial patients. Audio-only encounters for Medicare Advantage members must use the appropriate telephone E/M code (99441-99443).
What is the CPT code for E/M?
Beginning March 1, 2020, and for the duration of the COVID-19 public health emergency, CMS will cover telephone evaluation and management (E/M) services (CPT codes 99441-99443). Many private payers are also covering telephone E/M services as telehealth services delivered using audio-only.
Does Medicare cover cost sharing for telephone E/M?
As noted above, most payers are waiving cost-sharing for telephone E/M services. Physicians may elect to waive cost-sharing for Medicare beneficiaries. However, Medicare will not cover the beneficiary’s cost-sharing and the service will be paid as usual.
When will the Z71.9 ICd 10 be released?
The 2022 edition of ICD-10-CM Z71.9 became effective on October 1, 2021.
What is Z71 in medical?
Z71- Persons encountering health services for other counseling and medical advice , not elsewhere classified
What is a Z00-Z99?
Categories Z00-Z99 are provided for occasions when circumstances other than a disease, injury or external cause classifiable to categories A00 -Y89 are recorded as 'diagnoses' or 'problems'. This can arise in two main ways:
Popular Posts:
- 1. what is the icd 10 cm code for 31. irritable bowel syndrome
- 2. icd 10 code for 250.01
- 3. what is the icd 10 pcs code for mcbride bunionectomy?
- 4. icd-10-pcs code for baclofen pump placement attempted
- 5. icd 10 code for chemo status
- 6. icd 10 code for shoulder pain in both
- 7. icd 10 code for contact dermatitis due to unspecified agent
- 8. icd 10 code for sequelae of mva
- 9. icd-10 code for speech delay in child
- 10. icd 10 code for multiple cardiac risk factor