What is the ICD 10 code for Kienböck disease of adults?
Kienböck's disease of adults. M93.1 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2019 edition of ICD-10-CM M93.1 became effective on October 1, 2018.
What are the symptoms of Kienbock's disease?
Kienbock's disease causes one of the bones in the wrist (lunate bone) to slowly break down due to low blood supply. This process is called osteonecrosis. Symptoms include pain, swelling, limited movement, and decreased grip strength. The symptoms usually start in adulthood, but can occur at any age.
What is Kienböck's disease of the wrist?
Kienböck's disease is a condition where the blood supply to one of the small bones in the wrist, the lunate, is interrupted. Bone is living tissue that requires a regular supply of blood for nourishment.
Is Kienbock's disease inherited?
There is currently no evidence that Kienbock's disease is inherited. However, the cause of Kienbock's disease is poorly understood. It is possible that unidentified genetic factors contribute to the development of the condition. [3]

What is an ICD-9 diagnosis code?
ICD-9-CM is the official system of assigning codes to diagnoses and procedures associated with hospital utilization in the United States. The ICD-9 was used to code and classify mortality data from death certificates until 1999, when use of ICD-10 for mortality coding started.
How many icd9 codes are there?
13,000 codesThe current ICD-9-CM system consists of ∼13,000 codes and is running out of numbers.
What is the ICD-9 code for celiac disease?
ICD-9-CM Diagnosis Code 579.0 : Celiac disease.
Are ICD-9 codes still used in 2021?
CMS will continue to maintain the ICD-9 code website with the posted files. These are the codes providers (physicians, hospitals, etc.) and suppliers must use when submitting claims to Medicare for payment.
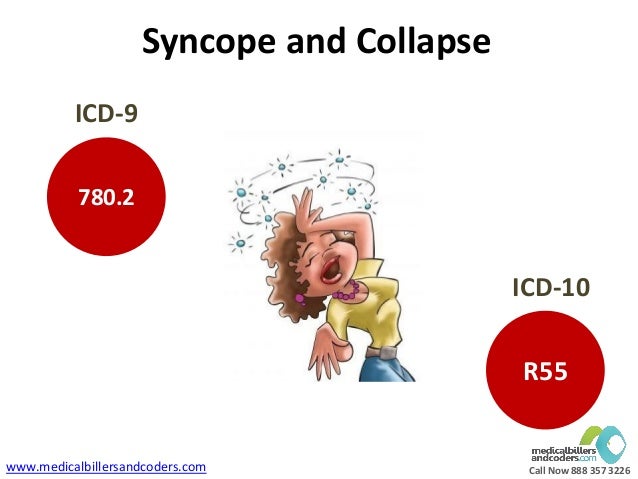
What is the difference between ICD-9 and ICD-10?
ICD-9 uses mostly numeric codes with only occasional E and V alphanumeric codes. Plus, only three-, four- and five-digit codes are valid. ICD-10 uses entirely alphanumeric codes and has valid codes of up to seven digits.
What are two difference between ICD-10 and ICD-9 coding?
The biggest difference between the two code structures is that ICD-9 had 14,4000 codes, while ICD-10 contains over 69,823. ICD-10 codes consists of three to seven characters, while ICD-9 contained three to five digits.
What is the ICD 10 code for celiac disease?
ICD-10 code K90. 0 for Celiac disease is a medical classification as listed by WHO under the range - Diseases of the digestive system .
What is an example of an ICD 9 code?
Most ICD-9 codes are three digits to the left of a decimal point and one or two digits to the right of one. For example: 250.0 is diabetes with no complications. 530.81 is gastroesophageal reflux disease (GERD).
What is International classification of Disease system?
The International Classification of Diseases (ICD) is a globally used diagnostic tool for epidemiology, health management and clinical purposes. The ICD is maintained by the World Health Organization (WHO), which is the directing and coordinating authority for health within the United Nations System.
When was ICD-9 discontinued?
Therefore, CMS is to eliminating the 90-day grace period for billing discontinued ICD-9- CM diagnosis codes, effective October 1, 2004.
When did ICD-9 go away?
CMS requires medical practices and RCM companies to make the switch from ICD-9 to ICD-10 by October 1, 2015, the last day for ICD-9 being September 30, 2015. This is not new. Organized, managed, and maintained by the World Health Organization, ICD codes are changed approximately once every 10 years.
When did ICD-9 stop?
No updates have been made to ICD-9 since October 1, 2013, as the code set is no longer being maintained.
What are the nonsurgical options for Kienbock's disease?
There are several nonsurgical and surgical options for treating Kienbock's disease. [6] . Nonsurgical options include keeping the wrist from moving and medications. Surgical options include restoring blood flow to the wrist and evening out the length of arm bones. The goals of treatment are to reduce pain, improve wrist movement, ...
How does Kienbock's disease get worse?
Kienbock's disease usually slowly gets worse over time. The underlying cause of Kienbock's disease is unknown. Diagnosis is made by imaging studies such as an MRI or CT scan. Treatment aims to relieve pressure and restore blood flow within the bone, and includes both surgical and non-surgical methods. [1] [2] [3]
What is the name of the bone that breaks down when you get Kienbock's disease?
Listen. Kienbock's disease causes one of the bones in the wrist (lunate bone) to slowly break down due to low blood supply. This process is called osteonecrosis. Symptoms include pain, swelling, limited movement, and decreased grip strength. The symptoms usually start in adulthood, but can occur at any age.
Does Kienbock's disease change over time?
Joint swelling. It is not well understood how Kienbock's disease changes over time. Most people start to develop symptoms in early adulthood. Typically, only one wrist is affected. Over time, the wrist joint may break down leading to arthritis in the surrounding bones.
How long do you have to wait to see a doctor for Kienböck's disease?
Kienböck's disease is a condition that progresses slowly, and many people do not decide to see a doctor until they have lived with symptoms for several months, perhaps longer. During your first appointment, your doctor will discuss your symptoms and medical history, then examine your hand and wrist.
Can you have more than one procedure for Kienböck's disease?
Some patients may require more than one procedure if the disease continues to progress. In summary, patients with Kienböck's disease should not expect to ever return to normal wrist function after any treatment. However, treatment gives the greatest opportunity for long-term preservation of function and pain relief.
Can a doctor diagnose Kienböck's disease?
In its early stages, Kienböck's disease may be difficult for your doctor to diagnose because the symptoms are so similar to those of a sprained wrist . Imaging tests, such as x-rays and magnetic resonance imaging (MRI) scans, are used to confirm a diagnosis of Kienböck's disease.
Is there a cure for Kienböck's disease?
Although there is no complete cure for Kienböck's disease, there are several nonsurgical and surgical options for treating it. The goals of treatment are to relieve the pressure on the lunate and to try to restore blood flow within the bone.
Can Kienböck's cause a sprained wrist?
The cause of Kienböck's disease is not known. Many people with Kienböck 's disease think they have a sprained wrist at first. They may have experienced some form of trauma to the wrist, such as a fall. This type of trauma can disrupt the blood flow to the lunate. Some things may put you more at risk for the disease.
Popular Posts:
- 1. icd 10 code for childhood obesity
- 2. icd-10-cm code for 2 - 1.5 cm lacerations of r 3rd finger
- 3. icd 10 code for continuous dependency of alcohol
- 4. icd 10 code for hx of blood transfusion
- 5. icd-10 code for trisomy 21
- 6. icd 10 code for infection due to foley catheter
- 7. icd 9 code for aftercare hypospadias repair
- 8. icd 10 code for chest p[ain
- 9. icd 10 cm code for abdominal gases
- 10. icd 10 code for geographic atrophy